
Elizabeth's Wish
Better Dementia Care, Safer Hospitals
What Is Elizabeth’s Wish?
Elizabeth’s Wish is a national policy proposal calling for mandatory dementia-safe standards in every NHS hospital.
The aim is simple: ensure that people with dementia receive safe, compassionate, accountable care wherever they are admitted.
The policy focuses on:
Mandatory dementia-specific staff training // Clear accountability and governance // Carer involvement as partners in care // Dementia-safe environments // Monitoring, reporting, and national standards
This isn’t about criticising staff, it’s about fixing the system they work in.

Why Change Is Urgent
People with dementia make up 1 in 4 hospital beds in the UK. Yet hospitals remain some of the least dementia-equipped environments.
This leads to:
Avoidable harm and distress // Falls, injuries, and infections // Delirium and accelerated decline // Poor communication with families // Longer hospital stays and higher readmission rates // Devastating human consequences, including preventable deaths
Elizabeth, like so many others, fell through these cracks.
The system didn’t fail because people didn’t care.
It failed because there were no systems.
982,000
It’s estimated that 982,000 people are living with dementia in the UK (2024) [1]
England recorded 482,978 people with a formal dementia diagnosis in Dec 2024 [2]
A significant proportion of all unscheduled hospital admissions involve people living with dementia [3]
NICE guidance states hospitals must adapt environments, communication, and care plans for people with dementia, yet compliance is inconsistent nationwide [4]
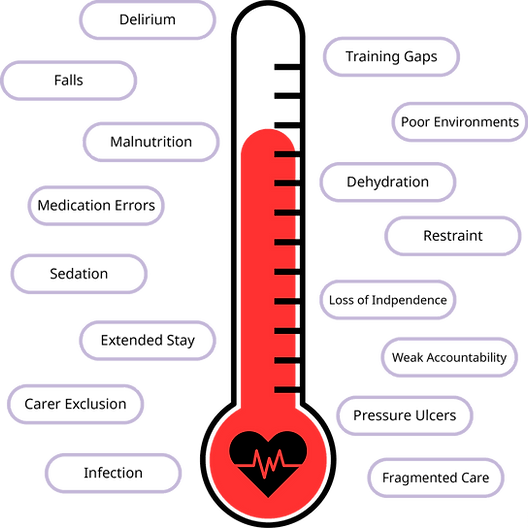
What’s going wrong?
National reviews show gaps in:
-
Staff training (clinical and non-clinical)
-
Environmental safety
-
Communication with families
-
Early detection of delirium
-
Understanding behavioural distress
-
Consistent accountability across Trusts
Impacts of inadequate dementia care:
People living with dementia face higher rates of:
-
Delirium
-
Falls
-
Use of restraints or sedatives
-
Poor nutrition and hydration
-
Longer lengths of stay
-
Family distress and loss of trust
[1] Alzheimer’s Society – Prevalence 2024 https://www.alzheimers.org.uk
[2] NHS England – Dementia Diagnosis Monthly Stats 2024 https://digital.nhs.uk/data-and-information
[3] NHS England – Dementia and Hospital Care https://www.england.nhs.uk
[4] NICE Guideline NG97 – Dementia Assessment, Management and Support https://www.nice.org.uk/guidance/ng97[5] NICE and HEE Dementia Training Standards Framework https://www.skillsforhealth.org.uk
Elizabeth’s Story
Elizabeth was admitted to hospital for care.
Instead, she encountered noise, confusion, lack of communication, and poor dementia-aware practice.
Her family were shut out instead of involved. Her needs were misunderstood instead of supported. Her safety was assumed instead of ensured.
She died because the hospital was not prepared to care for someone with dementia.
Her family vowed that her story must lead to change.
Elizabeth’s Wish is that change.
What if the system meant to protect your loved one actually puts them at risk?
People living with dementia face higher hospital risks when compared to other patients, meaning they are more likely to experience:
What We Are Asking the Government to Do
We are calling on the UK Government to implement a national, mandatory framework to ensure dementia-safe hospital care, including:
Tiered dementia training for all hospital staff // Board-level responsibility for dementia care quality // National standards and inspection for dementia care // Carer involvement rights // Safe environments and pathways designed for cognitive impairment // Data, reporting, and accountability for outcomes
This is achievable. Evidence-based. And urgently needed.
Improving dementia care does not require reinventing the system, it requires aligning what we already know works into a clear, coordinated pathway. The actions needed are simple, evidence-based, and achievable. By organising these steps into a national approach, we can deliver safer, more consistent, and more dignified care for people living with dementia.
The Pathway to Change

How You Can Help
Change won’t happen without public support.
Every signature, every share, every conversation moves this forward.
Sign the official Government petition
Share the campaign on X, Facebook & LinkedIn
Tell your story or the story of a loved one
Your voice could protect someone else’s grandmother, father, friend, or partner.
A Movement Rooted in Love and Accountability
Elizabeth’s Wish is more than a policy proposal.
It is a promise
No family should experience what Elizabeth’s family did.
No one with dementia should be unsafe in a hospital.
No preventable harm should ever be accepted as inevitable.
Together, we can make hospitals safer.
Together, we can make Elizabeth’s Wish a reality.
Meet The Author
Nathan is a HCPC registered paramedic with over 12 years of frontline experience as an
ambulance clinician, delivering care across diverse emergency and urgent care settings. He has a
strong professional and personal commitment to dementia care, informed by both clinical
experience and lived experience with the condition.
Nathan graduated with a First-Class Honours degree from the University of Cumbria, where his
research and critical analysis-based dissertation titled “Unlocking Innovation: Navigating Pre-
hospital Dementia Care with Assistive Technology - A Comprehensive Review of the
implementation and uses of Assisted Technology for Enhancing Pre-hospital Dementia Care”
focused on the pre-hospital assessment and care of people living with dementia, highlighting the
importance of early recognition, tailored interventions, and safe transitions into hospital care.
A dedicated dementia advocate, Nathan works to improve awareness, training, and standards
within the ambulance service, ensuring that people with dementia and their families receive safe,
compassionate and dignified care. Through his combined expertise in frontline practice, research,
and advocacy, Nathan seeks to influence policy and practice to enhance outcomes for patients
living with cognitive impairment.